Codman’s Triangle
Other Known Aliases – none
Definition – triangular area of new subperiosteal bone that is created when a bone tumor raises the periosteum away from the healthy bone
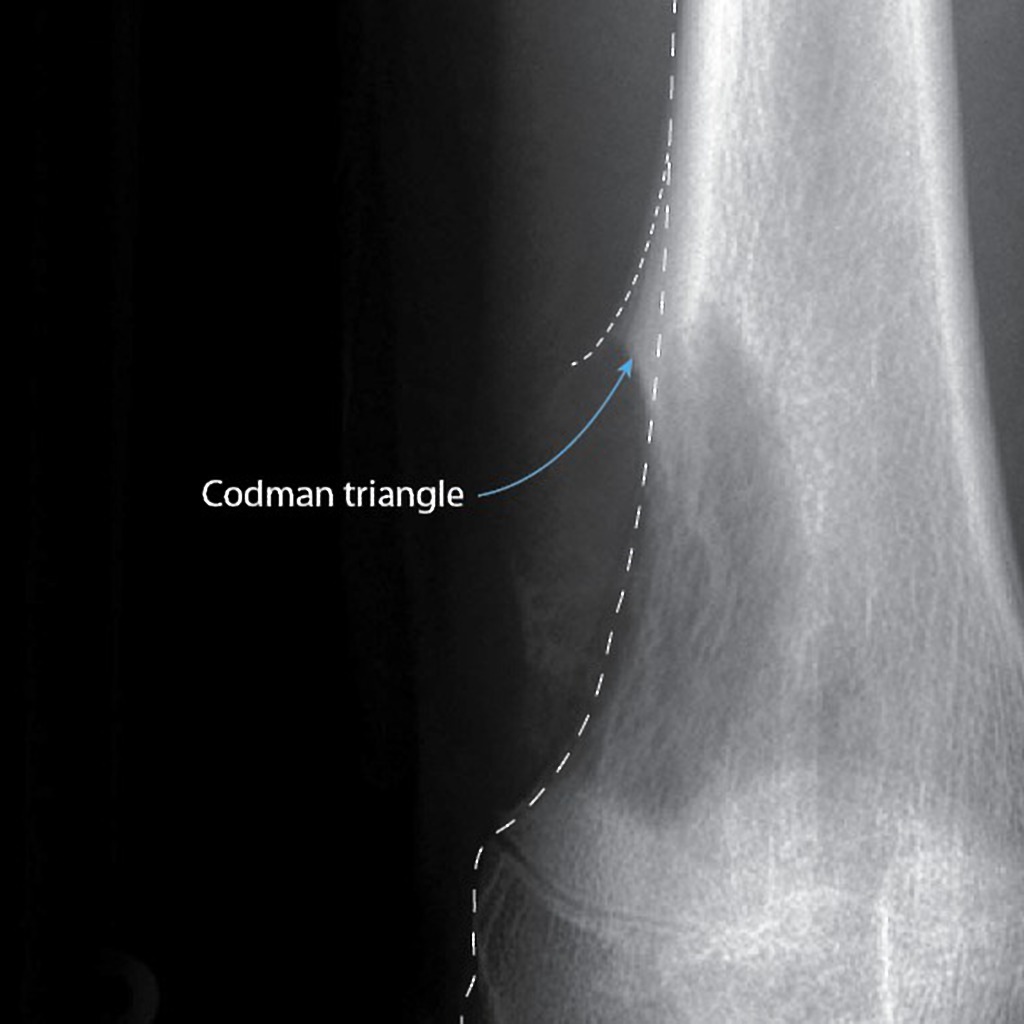
Clinical Significance – this occurs because the tumor is growing at a faster rate than the periosteum can expand, which leads to the periosteum tearing away and providing a second edge of ossification (thus making the triangle). Presence of this finding is highly suggested of a fast growing, malignancy.
History – Names after Ernest Amory Codman (1869-1940), who was an American surgeon and received his medical doctorate from Harvard University in 1895. Aside from being an accomplished surgeon, he fought for hospital reform and was an early adopter and advocate for patient-based outcomes. In fact, he created “End Result Cards” for his patients which included all diagnosis, procedures, and treatment for every one of his patients that he tracked for at least one year. He was also the first physician at Massachusetts General Hospital to institute a morbidity and mortality conference. Unfortunately, he lost his surgical privileges when he wanted to institute a plan for evaluating surgical competence. He went on to found his own hospital based on end-results and published these findings to the general public in 1916. He established the first bone tumor registry in the US and helped lead the founding of the American College of Surgeons and its Hospital Standardized Program, which eventually became the Joint Commission on Accreditation of Healthcare Organizations.
References
- Firkin BG and Whitwirth JA. Dictionary of Medical Eponyms. 2nd ed. New York, NY; Parthenon Publishing Group. 1996.
- Bartolucci S, Forbis P. Stedman’s Medical Eponyms. 2nd ed. Baltimore, MD; LWW. 2005.
- Yee AJ, Pfiffner P. (2012). Medical Eponyms (Version 1.4.2) [Mobile Application Software]. Retrieved http://itunes.apple.com.
- Whonamedit – dictionary of medical eponyms. http://www.whonamedit.com
- Up To Date. www.uptodate.com
- A Study in Hospital Efficiency. Boston : Privately printed, 1916.
- Bone Sarcoma, an Interpretation of the Nomenclature Used by the Committee of the Registry of Bone Sarcoma of the American College of Surgeons. New York : P. B. Hoeber, 1925.