What is it?
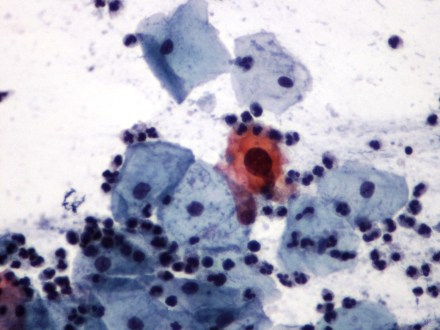
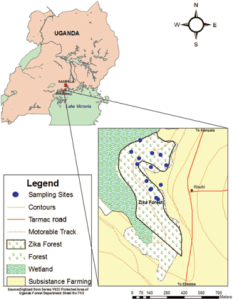
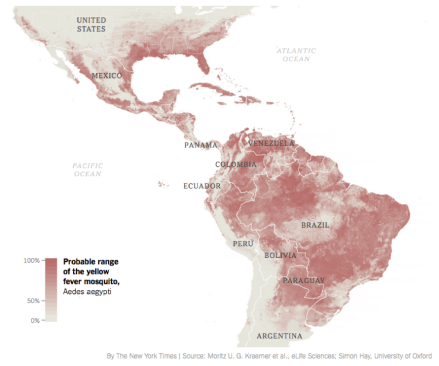
The Zika virus is a flavivirus that is related to yellow fever, dengue fever, West Nile, and Japanese encephalitis. It was first discovered in 1947 in a rhesus monkey and is called “Zika” because it originated in the Zika forest in Uganda. It is transmitted by the Aedes species of mosquitoes (which also carries dengue, chikungunya, and yellow fever).
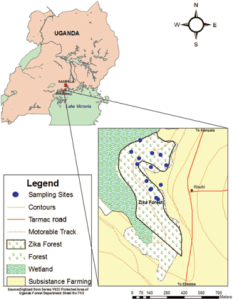
Kaddumukasa MA. J of Medical Entomology. 2014;51(1):104-113
Whats with all the noise?
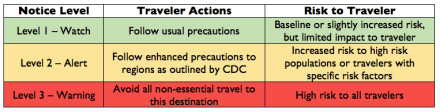
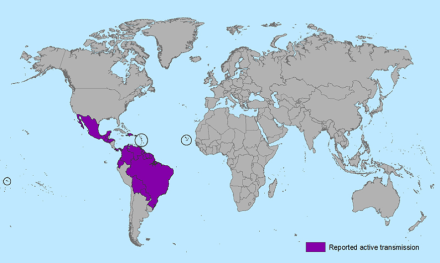
In May 2015, the Pan American Health Organization (PAHO) issued an alert regarding the first confirmed Zika virus infection in Brazil. Since then, there have documented cases of Zika virus infections in 20 countries in North and South America. Due to the threat and concern of transmission, the Center for Disease Control (CDC) issued a travel alert (Level 2-Practice Enhanced Precautions) for anyone traveling to these regions (see current list here).
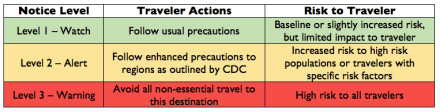
CDC Travel Alert Notice
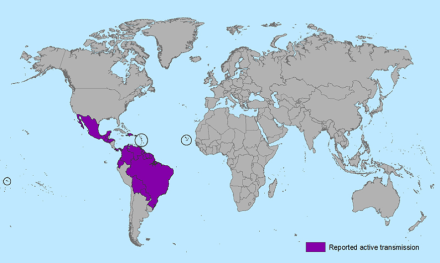
CDC Map of Reported Active Transmission
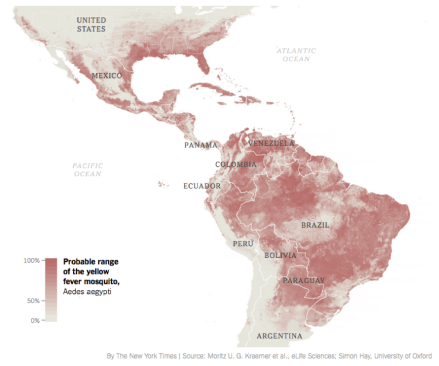
McNeil DG. SHort Answers to Hard Questions About Zika. New York Times. 2016
Signs and Symptoms
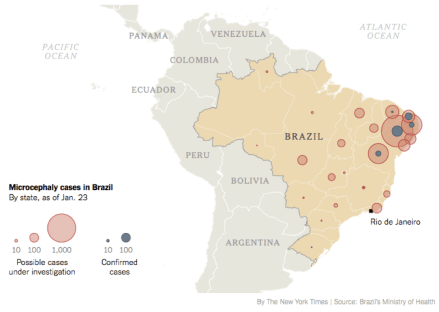
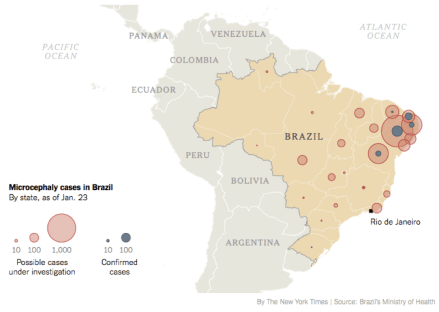
Only 1 in 5 people who become infected by the Zika virus develop symptoms, which are usually a mild viral prodromal syndrome (fever, rash, arthralgias, myalgias, conjunctivitis). Serious manifestations can include Guillaine-Barre syndrome and congenital microcephaly. Brazil has seen a 20-fold increase in number of cases of microcephaly from 2010 to 2014. Since October 2015, there have been 4,180 suspected cases (average of ~150/yr) of microcephaly in Brazil, but only 700 mothers were tested for the virus with only 270 positive results. The first case of microcephaly associated by the Zika virus on US soil was in Hawaii on January 15th, 2016 to a mother who lived in Brazil.
McNeil DG. Short Answers to Hard Questions About Zika. New York Times. 2016.
Because of the surge of microcephaly cases in an endemic region of Zika, the CDC is recommending that women who are pregnant, or are trying to become pregnant, should post-pone any travel to these regions.

McNeil DG. Short Answers to Hard Questions About Zika. New York Times. 2016.
Testing
Signs and symptoms of the acute Zika infection are very non-specific and the list of differential diagnoses is broad. If a patient has any suspicious symptoms within one week of travel to any of the at-risk regions, testing should occur as the Zika virus has become a nationally notifiable condition by the CDC. Testing includes reverse transcriptase-polymerase chain reaction (RT-PCR), virus-specific IgM and neutralizing antibodies and are only performed at the CDC Arbovirus Diagnostic Laboratory. Clinicians should contact local health departments to facilitate obtaining the correct testing sample and expediting transfer to the lab.
Treatment and Prevention
There is no specific treatment for the Zika virus. Treatment plans should be directed towards symptom relief and includes rest, oral rehydration, and acetaminophen for fever and pain relief. Aspirin and other NSAIDs should be avoided until dengue fever can be ruled out to decrease the risk of hemorrhage.
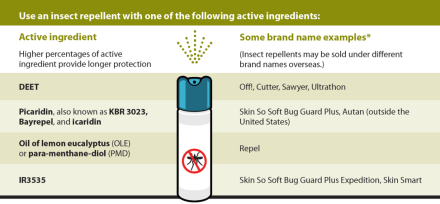
If travel must occur to endemic regions, patients should be advised to follow strict mosquito precautions to try to limit the exposure from the Aedes vector. N,N-Diethyl-meta-toluamide (DEET), Picaridin, oil of lemon eucalyptus, and IR3535 are all recommended by the CDC and are safe in pregnancy. There is no vaccine to the Zika virus yet, but preliminary works seem to be promising and early reports are pointing to the end of 2016 as a reasonable estimate for human trials to start.
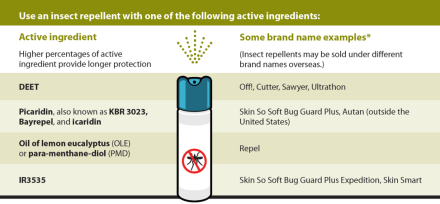
CDC Recommendations for Repellents
Bottom Line
For a PA practicing in the United States, this just adds to the list of traveler’s disease that you have to be hypervigilant about in patients with general complaints and recent travel to endemic regions. By no means do we need to start screening every patient with viral symptoms for Zika. But…if your patient has traveled to these regions, is pregnant, or may come into contact with patients who are pregnant, you should contact your local health department and screen them appropriately now that it is a nationally reportable disease. You should also take appropriate quarantine precautions if your clinic/department also has pregnant patients to limit disease contact to the most at risk patients. To date, there are no direct transmission cases of the virus (only the Aedes vector), but viruses can shift fast and it is better to be safer than sorry.
References
- Lucey DR, Gostin LO. The Emerging Zika Pandemic: Enhancing Preparedness. Published online January 27, 2016. doi:10.1001/jama.2016.0904.
- Kaddumukasa MA, Mutebi JP, Lutwama JJ, Masembe C, Akol AM. Mosquitoes of Zika Forest, Uganda: Species Composition and Relative Abundance. J of Medical Entomology. 2014;51(1):104-113.
- (2016, January 29). In Wikipedia, The Free Encyclopedia. Retrieved 17:33, January 31, 2016, from https://en.wikipedia.org/w/index.php?title=Aedes&oldid=702307969
- Zika virus. Centers for Disease Control and Prevention Available at: http://www.cdc.gov/zika/. Accessed February 1, 2016.
- Areas with Zika. Centers for Disease Control and Prevention Available at: http://www.cdc.gov/zika/geo/index.html. Accessed February 1, 2016.
- Brazil: 270 of 4,180 suspected microcephaly cases confirmed. The Big Story. Available at: http://bigstory.ap.org/article/25bba65de82b437080bedd4f9e229280/brazil-270-4120-suspected-microcephaly-cases-confirmed. Accessed February 1, 2016.
- Mcneil DG, Louis CS, St N. Short Answers to Hard Questions About Zika Virus. The New York Times Available at: http://www.nytimes.com/interactive/2016/health/what-is-zika-virus.html. Accessed February 1, 2016.
- Diagnostic Testing. Centers for Disease Control and Prevention Available at: http://www.cdc.gov/zika/hc-providers/diagnostic.html. Accessed February 1, 2016.
- Could We Have a Zika Vaccine Soon? NBC News. Available at: http://www.nbcnews.com/storyline/zika-virus-outbreak/could-we-have-zika-vaccine-soon-n507186. Accessed February 1, 2016.
- The Brazilian Doctors Who Sounded the Alarm on Zika and Microcephaly. WSJ. Available at: http://www.wsj.com/articles/the-brazilian-doctors-who-sounded-alarm-on-zika-and-microcephaly-1454109620?mod=e2tw. Accessed February 1, 2016.