Question
For celiac disease:
- What is the SCREENING serology test of choice?
- What is the CONFIRMATORY test of choice?


Question
For celiac disease:

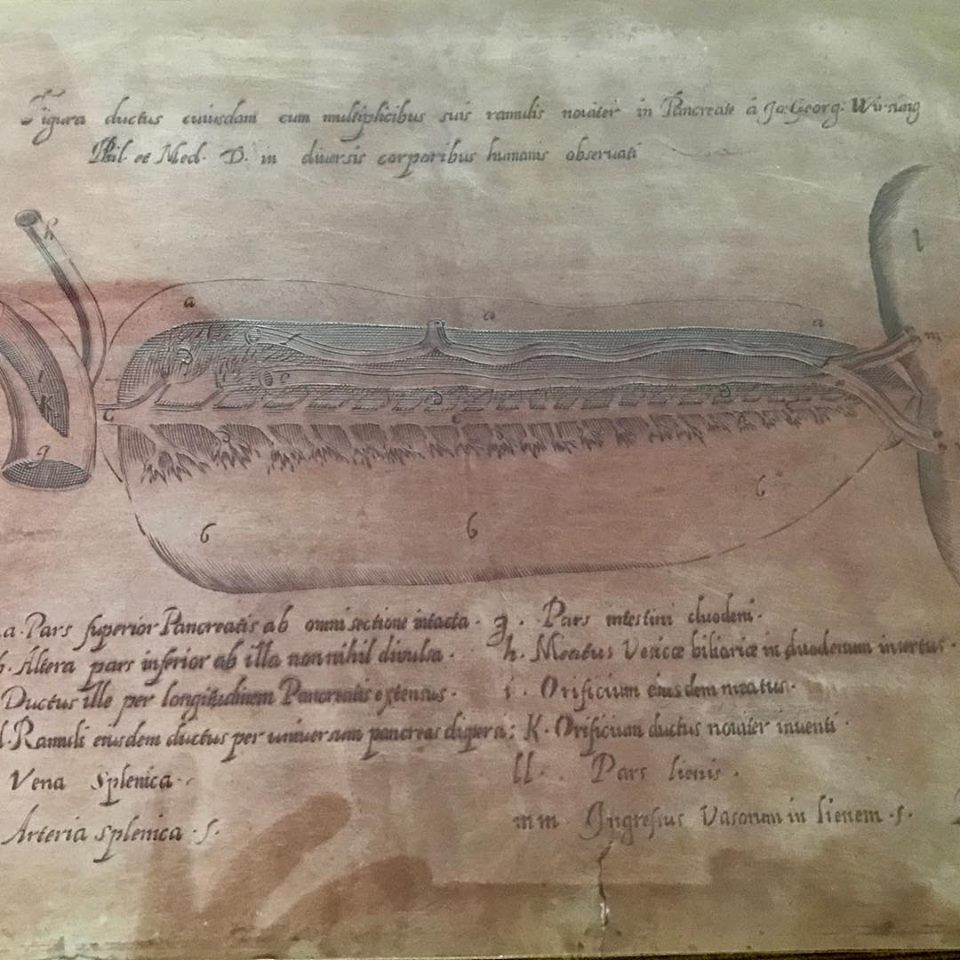
Duct of Wirsung
Other known aliases – main pancreatic duct
Definition – This is the main pancreatic duct that joins the pancreas to the common bile prior to the ampulla of Vater before emptying into the second portion of the duodenum

Clinical Significance – Having a single, major pancreatic duct is the most common anatomic variant for pancreatic anatomy, but some individuals may have an accessory duct that could be functional. The issue with this, of course, is management of pancreatic pathology so imaging may be required prior to instrumentation or surgical management.
History – Named after Johann Georg Wirsung (1589-1643), who was a German anatomist from Padua. He made this discovery while dissecting a criminal (Zuane Viaro) who was recently hanged for murder in 1642. Instead of formally publishing his findings, he engraved the sketch on a copper plate so numerous casting could be made and sent to the leading anatomists of the time. This finding is not without controversy. One year after this discovery, Wirsung was murdered in his house late at night by a Belgian student named Giacomo Cambier over a quarrel of first discovered this duct. In a cruel twist of fate, 5 years after his death, one of Wirsung’s students who was assisting in the dissection, Moritz Hoffman, claimed it was he who discovered this duct in a turkey rooster a year before Wirsung.

References
What vitamins have a higher potential for causing toxicity and why?
Fat soluble vitamins can be stored in the adipose tissue instead of excreted if in excess. As a result, vitamins A, D, E, and K can cause toxicity if patients take too much (in this order of incidence as well).

Morison’s Pouch
Other known aliases – hepatorenal recess/fossa, right posterior subhepatic space
Definition – a potential space between the liver and the right kidney
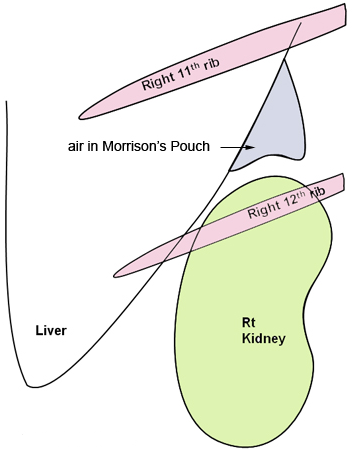
Clinical Significance – This a space where fluid can accumulate in the setting of ascites or abdominal trauma and be seen on CT or ultrasound. It is one of the view of a Focused Assessment of Sonography in Trauma (FAST) exam. Typically, 30-40mL of fluid needs to be present to be visualized.
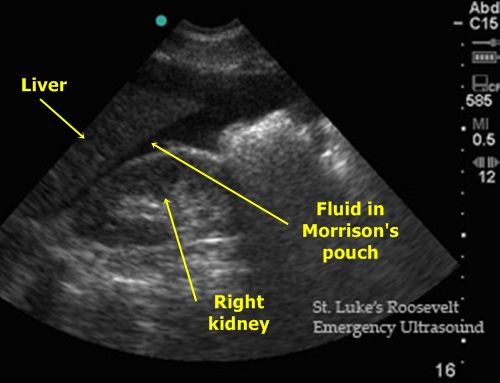

History – Named after James Rutherford Morison (1853-1939), a British surgeon who received his medical degree from the University of Edinburgh in 1874. He was also an assistant and “surgical dresser” for Joseph Lister early in his career and later founded a school of surgery at the University of Durham where he made his name as a prolific instructor of surgery. He is well known as a pioneer of modern surgery with several of his contemporaries noting he was twenty years ahead of his time and was a driving force of he surgical arts in Great Britain at the turn of the 20th century.
References
What vitamins have a higher potential for causing toxicity and why?

Other Known Aliases – pharyngeal diverticulum
Definition – sac-like outpouching of the mucosa and submucosa through Killian’s triangle, which is the area of structural weakness between the cricopharyngeus and lower inferior constrictor muscles.

Clinical Significance – There are actually three different types of diverticulae that can form in this region and are based on anatomic location:
Signs and symptoms of a Zenker’s diverticulum are pretty awful and include dysphagia, pulmonary aspiration, and halitosis from partially rotting food in the outpoaching. It is diagnosed via barium swallow under flouroscopy. The majority of the patients are male and present after the age of 60. Management is surgical resection.
History – Named after Friedrich Albert von Zenker (1825-1898), who was German physician and pathologist and received his medical doctorate at Leipzig in 1851. He held numerous teaching posts including chief prosector and professor of general pathology and anatomy at Dresden city hospital. Dr. Zenker, along with Hugo Wilhelm von Ziemssen, published a case series and literature review on his eponymous diverticulum in 1867 entitled “Krankheiten des Oesophagus”. He also was the first to document and describe trichinosis in a girl who died in 1860, proving that the once thought harmless parasite could cause severe disease.
References
Other Known Aliases – Inguinal triangle, medial inguinal fossa
Definition – Anatomical region of the abdominal wall outlined by the boundaries of the lateral margin of the rectus sheath, the inferior epigastric vessels, and the inguinal ligament.

Clinical Significance – The area is where direct hernias protrude through the abdominal wall.

History – Named after Franz Kasper Hesselbach (1759-1816), who was a German physician, surgeon, and anatomist in Hammelburg, Germany. He had a prolific career surgical assistant and prosector under Karl Kasper von Siebold at The Juliusspital in Würberg, before obtaining his doctor of medicine there. He is best known for his contributions to the surgery of hernias and has several other eponyms as well: Hesselbach’s fascia (cribriform fascia) and Hesselbach’s ligament (interfoveolar ligament.
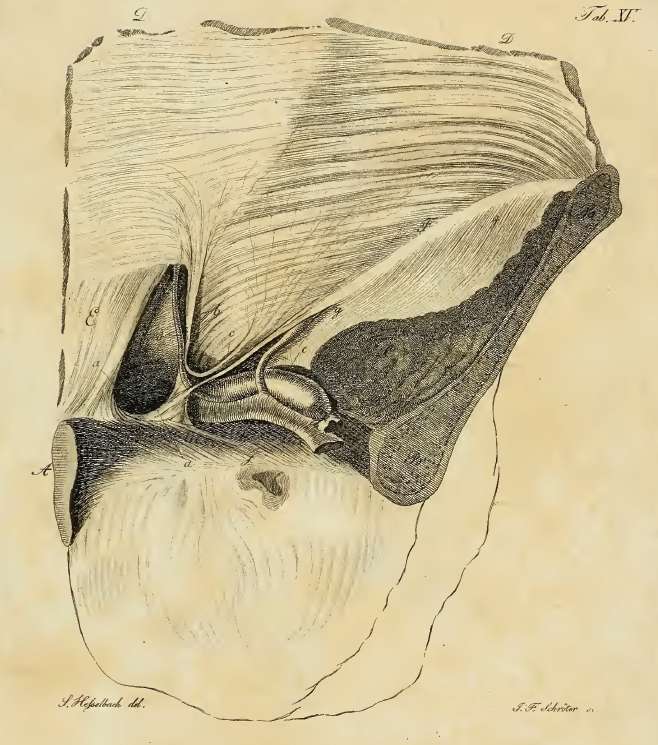
From his 1806 manuscript
References
What are the some of the pancreatitis scoring systems that are commonly used to estimate severity and mortality?
There are several scoring systems for estimating severity and mortality in pancreatitis.
References
Other Known Aliases – Moynihan’s Method (using just the thumb with patient supine)
Definition – Inspiratory arrest with deep palpation in the right upper quadrant
Clinical Significance – As the patient exhales, the abdominal organs move cephalad and under the diaphragm. After full exhalation and during inspration, the organs move caudal back into the abdominal cavity. When there is inflammation of the gallbladder, the patient will stop inhaling as the inflammed gallbladder touches the practitioner’s fingers during deep palpation of the right upper quadrant.
History – Named after John Benjamin Murphy (1857-1916), who was an American surgeon and early pioneer for many different surgical operations and techniques. In fact, William James Mayo (co-founder of The Mayo Clinic) called him “the surgical genius of our generation”.
In 1889, he advocated for and popularized early appendectomy in all suspected appendicitis cases and had over 200 successful cases to begin convincing his colleagues of the benefits of early surgery. Dr. Murphy also pioneered treatment of tuberculosis with iatrogenic pneumothoraces and was the first surgeon to re-anastomose a transected femoral artery from a gunshot wound. He was also a distinguished teacher and developed “wet clinics” at Mercy Hospital, where he operated and lectured to an audience of learners in a traditional operative theater.

Dr. Murphy also attended to Theodore Roosevelt after an assassination attempt and was one of the founding members of the American College of Surgeons. He is also the author of one of the more famous quotes pertaining to patient-centered care.
References