Loop of Henle
Other Known Aliases – ansa nephroni
Definition – portion of the nephron that goes from the proximal convoluted tubule to the distal convoluted tubule. There are four portions of this structure:
- Thin descending segment
- Thin ascending segment
- Ascending limb
- Cortical thick ascending limp

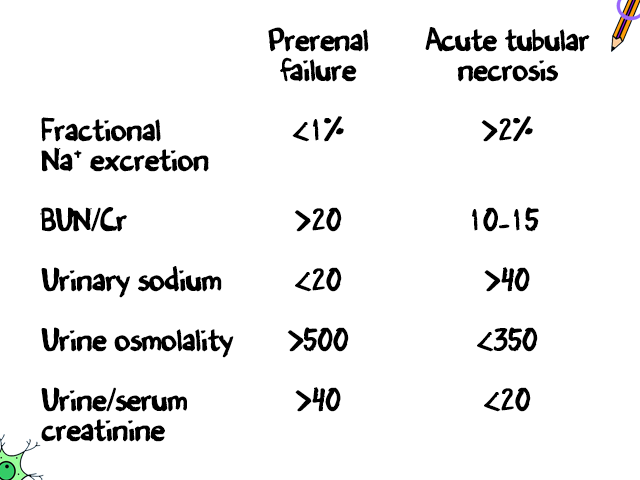
Clinical Significance – the loop of Henle creates an area of high urea concentration with secretion and reabsorption of water and electrolytes. This is also the portion of the nephron where the aptly named “loop diuretics” to manage blood pressure by means of excess fluid excretion.
History – Named after Friedrich Gustav Jakob Henle (1809-1885), who was a German physician, pathologist, and anatomist and received his medical doctorate from the University of Bonn in 1832. He spent his early career as a prosector for Johannes Müller in Berlin where he published furiously on numerous facets of human and animal anatomy and physiology. He then went on to become the chair of anatomy at the University of Zurich, where he became one of the early adopters and advocates for the study of pathophysiology as a single distinct discipline. He also set the early argument for the germ theory in an essay entitled “On Miasma and Contagia”. His life’s work culminated in the publishing of the Handbook of Systematic Human Anatomy in 1855, which was the most complete and comprehensive work at that time.
References
- Firkin BG and Whitwirth JA. Dictionary of Medical Eponyms. 2nd ed. New York, NY; Parthenon Publishing Group. 1996.
- Bartolucci S, Forbis P. Stedman’s Medical Eponyms. 2nd ed. Baltimore, MD; LWW. 2005.
- Yee AJ, Pfiffner P. (2012). Medical Eponyms (Version 1.4.2) [Mobile Application Software]. Retrieved http://itunes.apple.com.
- Whonamedit – dictionary of medical eponyms. http://www.whonamedit.com
- Up To Date. www.uptodate.com