Cardiovascular
Ep-PAINE-nym
Levine’s Sign
Other Known Aliases – Palm Sign, Cossio’s Sign, Cossio-Levine’s Sign
Definition – Clenched fist held over the sternum while a patient is describing their chest pain and classically is the right hand, as cardiac pain can refer to the left arm.

Clinical Significance – There is very little significance to this sign and has been studied to only have a 14% sensitivity for cardiac chest pain, but is a classic physical exam finding and frequent pimp fodder.
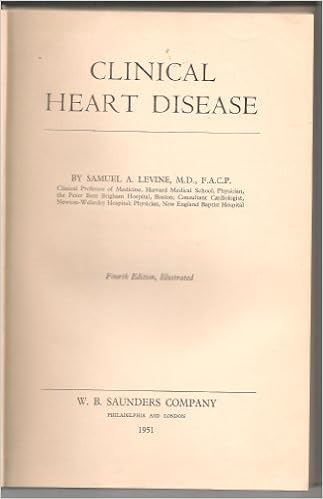
History – Named after Samuel Albert Levine (1891-1966), who was an American cardiologist and attending physician at The Brigham Hospital in Boston, MA, and assistant professor of medicine at Harvard University. He graduated Harvard at the age of 20 and was the first physician to diagnose President Franklin Roosevelt with poliomyelitis. He was a pioneer in coronary thrombosis research and was the second physician to ever diagnose the condition, which he described it in his classic book Clinical Heart Disease in 1936.

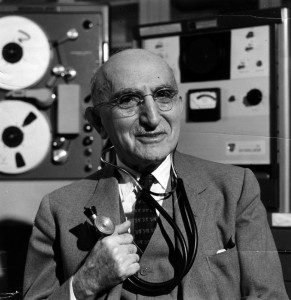
He is also the namesake of The Levine Scale, a 1 to 6 grading system to characterize the intensity of heart murmurs, and Lown-Ganong-Levine syndrome, which is a pre-excitation syndrome causing a shortened PR interval with normal QRS complexes in tachycardia.

The Levine Scale

Lown-Ganong-Levine Syndrome
References
- Firkin BG and Whitwirth JA. Dictionary of Medical Eponyms. 2nd ed. New York, NY; Parthenon Publishing Group. 1996.
- Bartolucci S, Forbis P. Stedman’s Medical Eponyms. 2nd ed. Baltimore, MD; LWW. 2005.
-
Yee AJ, Pfiffner P. (2012). Medical Eponyms (Version 1.4.2) [Mobile Application Software]. Retrieved http://itunes.apple.com.
- Whonamedit – dictionary of medical eponyms. http://www.whonamedit.com
-
Edmondstone WM. Cardiac chest pain: does body language help the diagnosis? BMJ. 1995;311(7021):1660-1. [pubmed]
- Levine HJ. Profiles in Cardiology: Samuel A. Levine (1891-1966). Clin Cardiol. 1992;15:473-476
-
Bedford DE. Samuel Albert Levine (1891-1966). British heart journal. 1966; 28(6):853-4. [pubmed]
-
Silverman ME, Wooley CF. Samuel A. Levine and the history of grading systolic murmurs. The American journal of cardiology. 2008; 102(8):1107-10. [pubmed]
-
Lown B, Ganong WF, Levine SA. The syndrome of short P-R interval, normal QRS complex and paroxysmal rapid heart action. Circulation. 1952; 5(5):693-706. [pubmed]
PAINE #PANCE Pearl – Emergency Medicine
Question
What are some of the chest scores we use to evaluate the likelihood a patient with chest pain is having ACS?

PAINE #PANCE Pearl – Emergency Medicine
Question
What are the 5 main life-threatening causes of chest pain?
Answer
The 5 main life-threatening causes of chest pain you should ALWAYS think of are:
- Acute Myocardial Infarction
- Pulmonary Thromboembolism
- Pneumothorax (risk of tension)
- Pericarditis (risk of tamponade)
- Aortic Dissection
There are a few others that should also cross your mind:
- Esophageal Rupture (Boerhaave’s Syndrome)
- Acute Chest Syndrome in Sickle Cell patients
- Unstable angina
References
- The Five Deadly Causes of Chest Pain Other than Myocardial Infarction. JEMS. 2017
- Chest Pain. Life in The Fastlane.
- Woods WA, Young JS, Just JS. Emergency Medicine Recall. 2000.
PAINE #PANCE Pearl – Cardiovascular
82-year-old male, with a history of HTN, HLD, and CAD, presents to your clinic with a six-month history of dyspnea on exertion. He states he is unable to walk as far as he used when exercising, and when he over exerts himself, he reports having some mild chest pain and feeling lightheaded. This resolves with rest and he denies any syncope with these events.
Medications
Metoprolol 50mg daily
Lisinopril 10mg daily
Simvastatin 30mg daily
Vital Signs
BP – 158/97
HR – 62
RR – 13
O2% – 100%
Physical exam
General – WN/WD male in NAD
Pulmonary – CTA without adventitial breath sounds
CV – Soft S2 with murmur over right 2nd intercostal space
PV – carotid pulse is weak and has a slow rise, murmur is appreciated
Neuro – No focal deficits
EKG
This patient has aortic stenosis. The suggestive parts of the H&P are:
- History
- The classic triad of aortic stenosis is chest pain, dyspnea, and syncope.
- Aortic stenosis increases in prevalence with age
- Cardiac Auscultation
- Peripheral Vascular
- EKG
- Shows LVH and strain pattern in precordial leads
- What is the next step in the management of this patient?
- Transthoracic echocardiography
- After the next step, what important variables must you specifically assess?
- Valvular anatomy and size
- Aortic valve surface area
- Valve hemodynamics
- Transvavular aortic velocity
- Mean transvalvular pressure
- LV size and ejection fraction
- Pulmonary artery pressure
- Other concomitant conditions
- Valvular anatomy and size
These variables will help with staging the severity of the stenosis, as well as determine need for operative intervention.
Ep-PAINE-nym
Bainbridge Reflex
Other known aliases – Atrial Reflex
Definition – Compensatory increase in heart rate caused by a rise in right atrial pressure. Opposite of carotid baroreceptors.
Clinical Significance – Respiratory sinus arrythmia. Inspiration causes increased venous return.
History – Described by Francis Arthur Bainbridge in 1915
References
-
Hakumäki MO. Seventy years of the Bainbridge reflex. Acta physiologica Scandinavica. 1987;130(2):177-85. [pubmed]
- Firkin BG and Whitwirth JA. Dictionary of Medical Eponyms. 2nd ed. New York, NY; Parthenon Publishing Group. 1996.
- http://www.healio.com/cardiology/learn-the-heart/cardiology-review/topic-reviews/bainbridge-reflex
PAINE #PANCE Pearl – Cardiovascular
82-year-old male, with a history of HTN, HLD, and CAD, presents to your clinic with a six-month history of dyspnea on exertion. He states he is unable to walk as far as he used when exercising, and when he over exerts himself, he reports having some mild chest pain and feeling lightheaded. This resolves with rest and he denies any syncope with these events.
Medications
Metoprolol 50mg daily
Lisinopril 10mg daily
Simvastatin 30mg daily
Vital Signs
BP – 158/97
HR – 62
RR – 13
O2% – 100%
Physical exam
General – WN/WD male in NAD
Pulmonary – CTA without adventitial breath sounds
CV – Soft S2 with murmur over right 2nd intercostal space
PV – carotid pulse is weak and has a slow rise, murmur is appreciated
Neuro – No focal deficits
EKG
Questions
- What is the next step in the management of this patient?
- After the next step, what important variables must you specifically assess?
#26 – Pericardial Effusion and Cardiac Tamponade
***LISTEN TO THE PODCAST HERE***
Anatomy
The pericardium consists of a double-layered semi-elastic sac that holds the heart in the mediastinum. Basically, so the heart doesn’t flop around inside the thoracic cavity. There should be a small amount of fluid (15-50mL) present to prevent adhesion of the pericardial sac to the heart. It is then termed an effusion when it is more than the normal amount. How much quantifies an effusion? Doesn’t matter…. what does matter is how fast that fluid develops. Because the pericardium is semi-elastic, it can accommodate and stretch over time if the accumulation is slow. This would lead to a greater volume of fluid before symptoms occur. If the fluid accumulates rapidly, less volume can produce profound effects due to the restrictive nature of the fibrous pericardium.
Etiology
- Infectious
- Viral
- Bacterial
- Fungal
- Parasitic
- Non-infectious
- Neoplastic
- Autoimmune/inflammatory
- Trauma
- Cardiac
- Radiation
- Metabolic
Signs and Symptoms
There are no reliable historical clues or physical exam findings that are specific to pericardial effusions. They are helpful, though, to sort out the cause of the effusion. Common findings include:
- Fever
- Dyspnea
- Chest pain
- Tachycardia
- JVD
- Hepatomegaly
- Pulsus paradoxus
-
- Ewart’s Sign
- Dullness to percussion, egophony, and bronchial breath sounds over the inferior angle of the left scapula
- Beck’s Triad
- Hypotension
- JVD
- Muffled heart tones
Work-Up
- EKG
- Sinus tachycardia
- Low voltage QRS (≤5mm in the 6 limb leads)
- Electrical alternans
-

Life In The Fastlane – o http://lifeinthefastlane.com/ecg-library/basics/low-qrs-voltage/
- Chest X-ray
- Small effusions are generally not appreciated on radiography
- Larger, chronic effusions may appear as an enlarged cardiac silhouette classically referred to as a “Water bottle heart”
- Echocardiogram
- Looking for anechoic stripe around the heart
- < 1cm ≈ 100cc
- 1-2cm ≈ 100-500cc
- > 2cm ≈ >500cc
- 2D Apical 4-chamber is my view of choice
- Severity can also be assessed by looking for:
- RV collapse during diastole
- LV collapse with increased EF
- IVC dilation and loss of respiratory variations
-
- Looking for anechoic stripe around the heart
Treatment
- Pericardiocentesis with catheter placement
-
- Three-way stopcock is used to measure pericardial pressure
- Fluid is then sequentially removed and pressure re-measured until < 5mmHg during inspiration
-
-
- Open surgical drainage via pericardial window if:
- Fluid accumulates after catheter drainage
- Effusion is loculated
- Need for biopsy
- Patient has coagulopathy
-
-
References
- Braunwald E. Pericardial Disease. In: Kasper D, Fauci A, Hauser S, Longo D, Jameson J, Loscalzo J. eds. Harrison’s Principles of Internal Medicine, 19e. New York, NY: McGraw-Hill; 2015. http://accessmedicine.mhmedical.com/content.aspx?bookid=1130&Sectionid=79743215. Accessed January 12, 2017.
- Imazio M. Contemporary management of pericardial diseases. Current Opinion in Cardiology. 2012;27(3):308-17. [pubmed]
- Levy PY, Corey R, Berger P. Etiologic diagnosis of 204 pericardial effusions. Medicine. 2003;82(6):385-91. [pubmed]
- Permanyer-Miralda G. Acute pericardial disease: approach to the aetiologic diagnosis. Heart (British Cardiac Society). 2004;90(3):252-4. [pubmed]
- Bruch C, Schmermund A, Dagres N. Changes in QRS voltage in cardiac tamponade and pericardial effusion: reversibility after pericardiocentesis and after anti-inflammatory drug treatment. Journal of the American College of Cardiology. 2001;38(1):219-26. [pubmed]
- Sternbach G. Claude Beck: cardiac compression triads. The Journal of Emergency Medicine. 1989;6(5):417-9. [pubmed]
- Stanford University. Tamponade. Echocardiography in ICU. https://web.stanford.edu/group/ccm_echocardio/cgi-bin/mediawiki/index.php/Tamponade.
- Adler Y, Charron P, Imazio M. 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC)Endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS). European Heart Journal. 2015;36(42):2921-64. [pubmed]
- Gumrukcuoglu HA, Odabasi D, Akdag S, Ekim H. Management of Cardiac Tamponade: A Comperative Study between Echo-Guided Pericardiocentesis and Surgery-A Report of 100 Patients. Cardiology Research and Practice. 2011:197838. [pubmed]
PAINE #PANCE Pearl – Cardiovascular
Question
What are the 3 eponymous physical exam findings in patients with bacterial endocarditis and who were they named after?
Answers
Osler Nodes
- Painful, erythematous nodules of the hands and feet
- Named after Sir William Osler in 1908.
Janeway Lesions
- Nontender, erythematous or hemorrhagic macular or nodular lesions on the palms or soles
- Named after Theodore Caldwell Janeway in the late 1800s.
Roth Spots
- Retinal hemorrhages with white or pale centers.
- Named after Swiss pathologist Mortiz Roth in 1872
References
- Osler W. Chronic Infectious Endocarditis. Quarterly Journal of Medicine. 1908;2:219-230.
-
Ruiz-García J, Canal-Fontcuberta I. Diagnosis of Active Infective Endocarditis from Examination of the Toes and Soles. The American Journal of Cardiology. 2016;118(7):1094. [pubmed]
-
Khanna N, Roy A, Bahl VK. Janeway lesions: an old sign revisited. Circulation. 2013;127(7):861. [pubmed]
-
Sethi K, Buckley J, de Wolff J. Splinter haemorrhages, Osler’s nodes, Janeway lesions and Roth spots: the peripheral stigmata of endocarditis. British Journal of Hospital Medicine. 2013;74(9):C139-42. [pubmed]
PAINE #PANCE Pearl – Cardiovascular
Happy 2017!!! I apologize for the delay in having the pearls coming out, but life is life. So here you go:
What are the 3 eponymous physical exam findings in patients with bacterial endocarditis and who were they named after?