Tail of Spence
Other Known Aliases – processus lateralis mammae
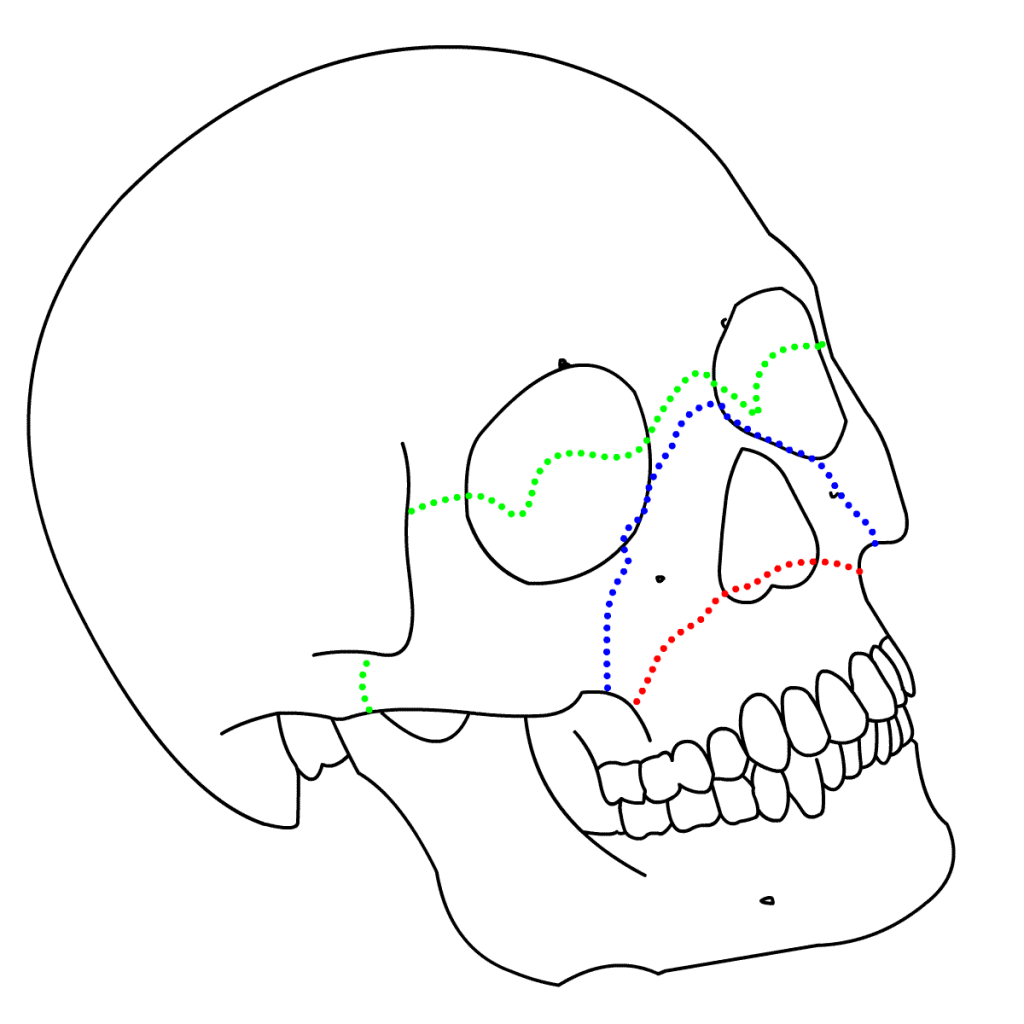
Definition – triangular, tongue-shaped portion of breast tissue that extends superiorly and laterally toward the axilla, perforating the deep axillary fascia where it terminating in close proximity to the axillary lymph nodes.

Clinical Significance – Due to location of this breast tissue, many women may not exam this portion of the breast during self-exams. Therefore, given its close proximity to the axillary lymph nodes, providers need to pay close attention to this anatomic region.

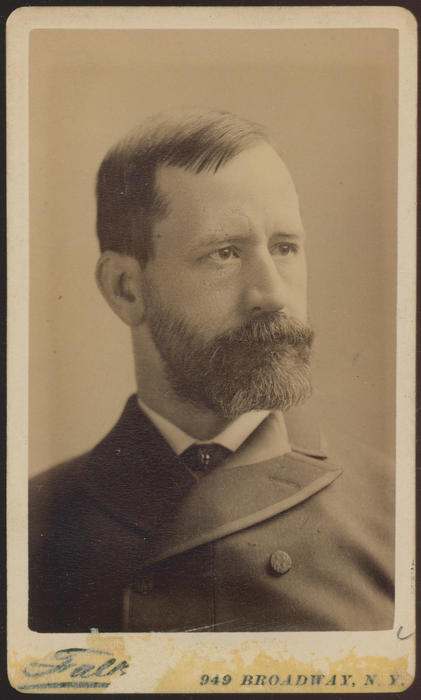
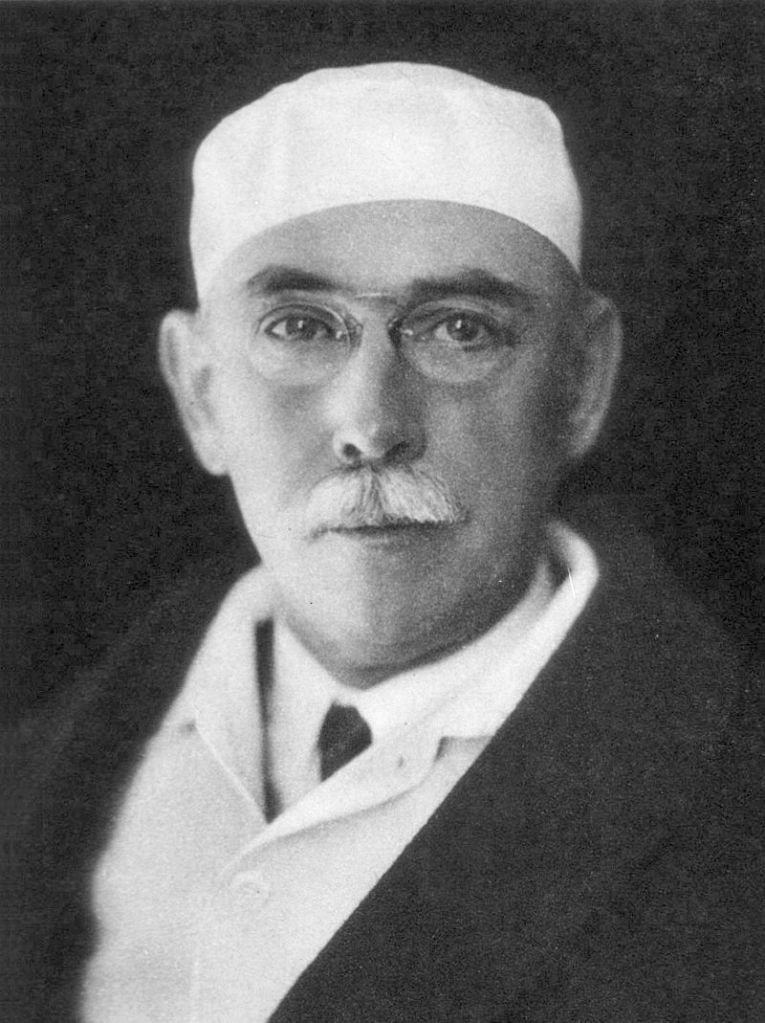
History – Named after James Spence (1812-1882), who was a Scottish surgeon and received his medical doctorate from the Royal College of Surgeons of Edinburgh in 1832. He went on to have a prolific career in teaching anatomy in the classroom and in the dissecting hall at various schools and universities, culminating in serving as chair of systematic surgery and Professor of Surgical Science at Edinburgh University in 1864. Clinically, he served as full house surgeon at the Edinburgh Royal Infirmary for many years leading up to his appointment as Surgeon in Ordinary to Queen Victoria in Scotland in 1865. He was elected as a Fellow of the Royal Society of Edinburgh in 1866 and served as president of the Royal College of Surgeons of Edinburgh from 1867-1869.

References
- Firkin BG and Whitwirth JA. Dictionary of Medical Eponyms. 2nd ed. New York, NY; Parthenon Publishing Group. 1996.
- Bartolucci S, Forbis P. Stedman’s Medical Eponyms. 2nd ed. Baltimore, MD; LWW. 2005.
- Yee AJ, Pfiffner P. (2012). Medical Eponyms (Version 1.4.2) [Mobile Application Software]. Retrieved http://itunes.apple.com.
- Whonamedit – dictionary of medical eponyms. http://www.whonamedit.com
- Up To Date. www.uptodate.com