Question
Ischemic bowel disease has two classic presentations: acute and chronic.
- What is the typical type of patient (or risk factors) for each?
- How does each type classically present?

Rovsign’s Sign
Other Known Aliases – none
Definition – palpation of the left lower quadrant causes perceived pain in the right lower quadrant
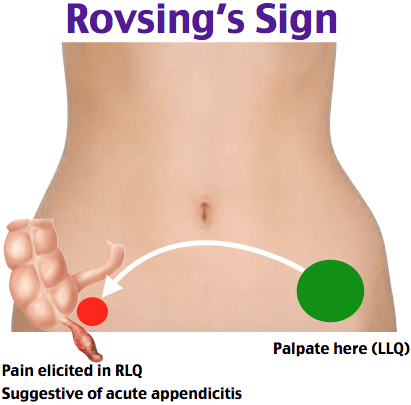
Clinical Significance – A positive Rovsing’s sign is suggestive of appendicitis. There are two mechanisms that illicit this response. First, palpation of the left lower quadrant stretch the peritoneal lining over the appendix and causes pain. Second, deep palpation of descending colon in the left lower quadrant causes the gas present to stretch the lumen of the colon and appendix causing pain.
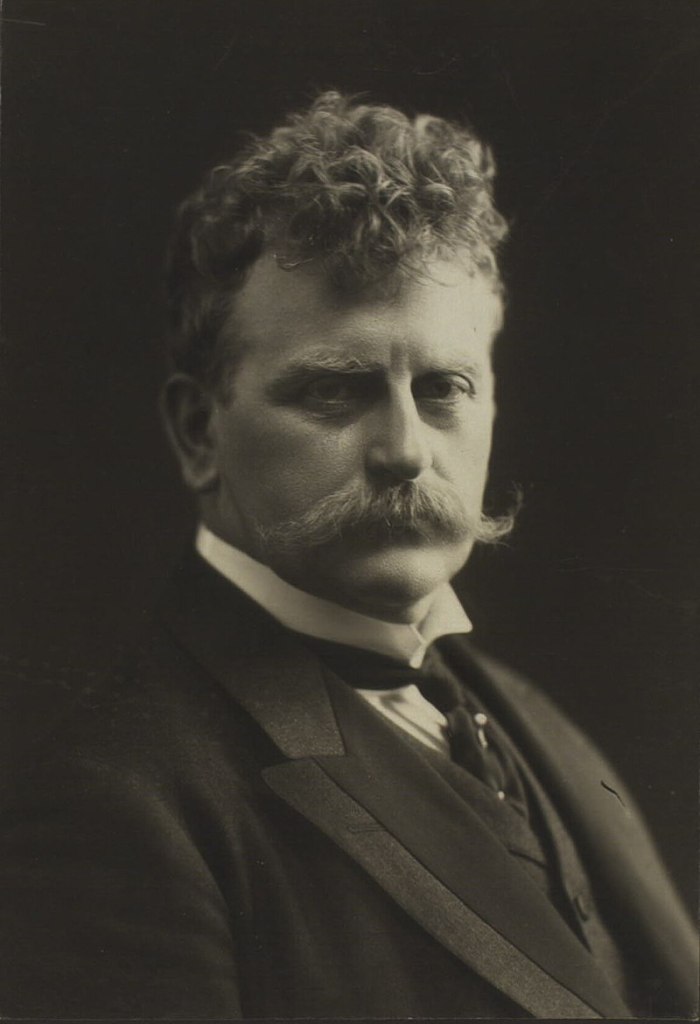
History – Named after Niels Thorkild Rovsing (1862-1927), who was a Danish surgeon and received his medical doctorate from the University of Copenhagen in 1885. He went on to become professor of operative surgery there in 1899, as well as chief surgeon at Louise-Børnehospital and Red Cross Hospital. He was a huge advocate for better surgical accommodations for patients, even going so far as to commission his own private surgical nursing home to care for his postoperative patients. He was international recognized as an accomplished abdominal surgeon, writing extensively on these surgical diseases. He first published his findings of his eponymous exam finding in 1907 in an article entitled “Indirect cause of typical pain at McBurney’s point”.
He also has several other surgical eponyms attributed to him including:
References
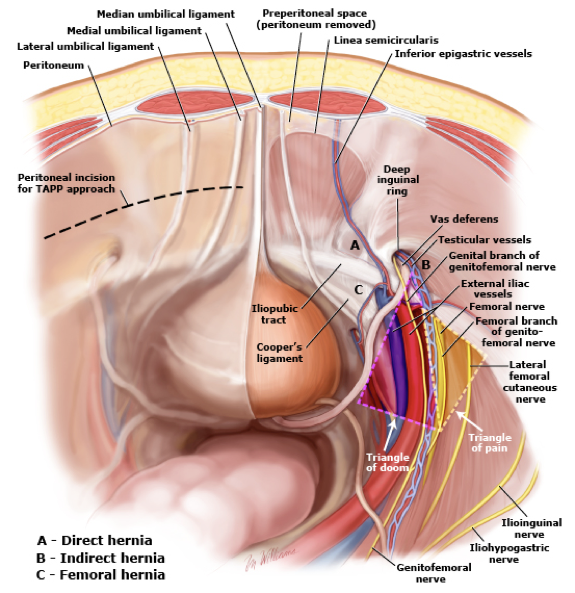
The abdominal wall is made up of multiple, overlapping muscles and connective tissue whose main purpose is to contain and protect the intra-abdominal organs, while also serving as accessary muscles of respiration and facilitating axial movements. The bony boundaries of the abdominal cavity are:
The lateral rectus abdominis muscles also fuse midline to form the linea alba and laterally to the connect with the confluence of the external oblique, internal oblique, and transverse abdominis muscles.
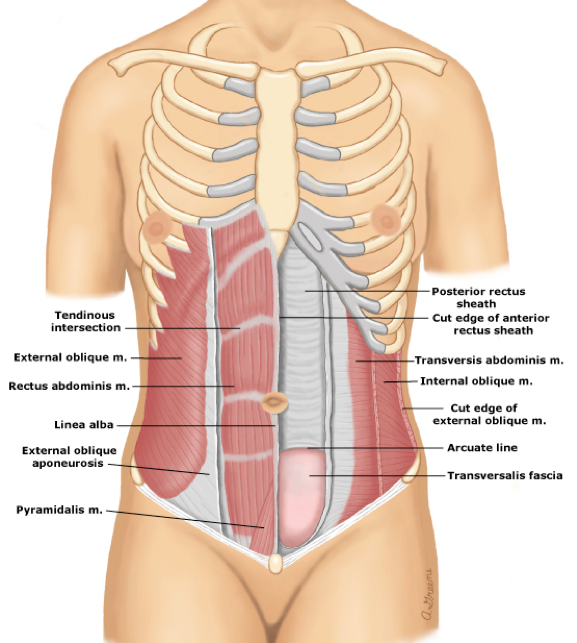
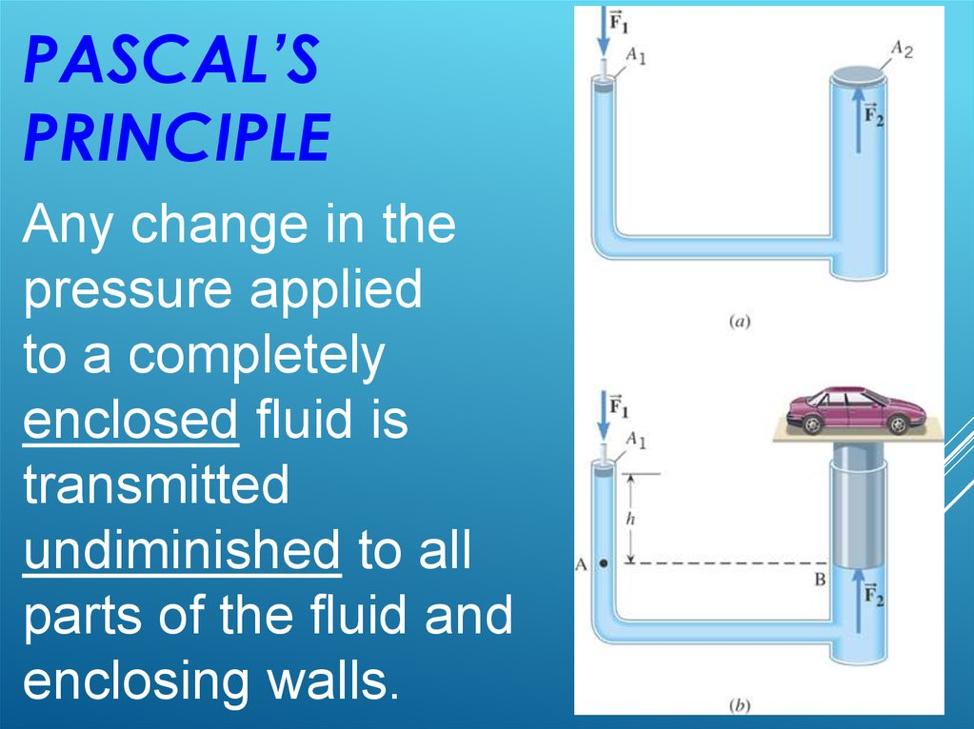
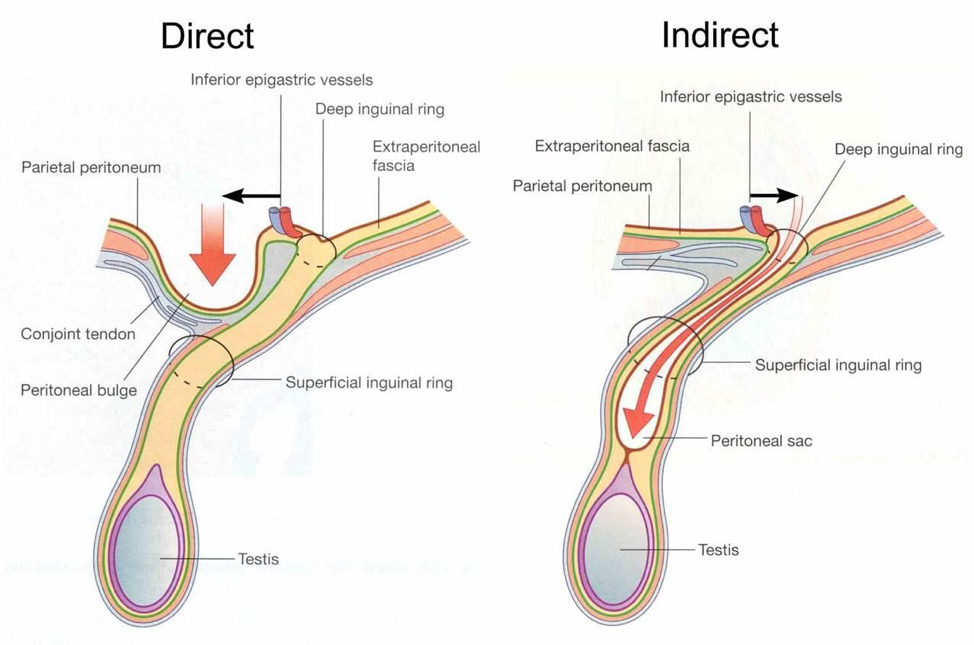
Weakness at any of these junctions (either anatomic or iatrogenic) can allow herniation of abdominal contents through this defect. Pascal’s principle states that any pressure generated within a closed system (abdominal cavity) is transmitted equally to the walls of the system.

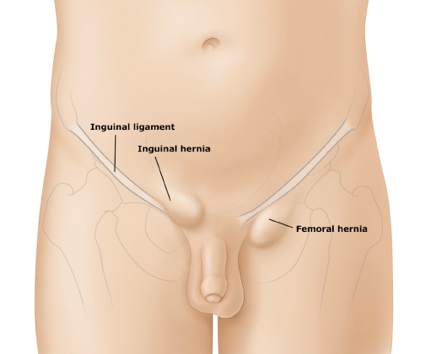


Most hernias in non-obese patients should be diagnosed by careful and thorough history and physical examination. In others, radiographic investigation must be performed.


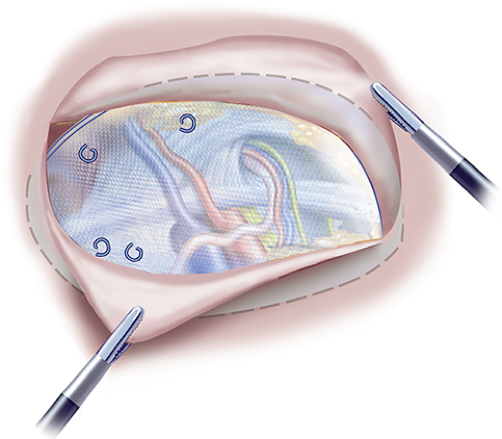
Most hernias will require surgical repair at some point. The decision for operative management comes down to risk of future complications, size, and symptom tolerance. Patients with strangulation or incarceration MUST emergent/urgent surgical repair to limit the risk of bowel ischemia.
Surgeon preference and patient considerations dictate laparoscopic vs open hernia repair.
Preclusion to laparoscopic repair include:

Hirschprung Disease
Other Known Aliases – congenital aganglionic megacolon, congenital intestinal aganglionosis
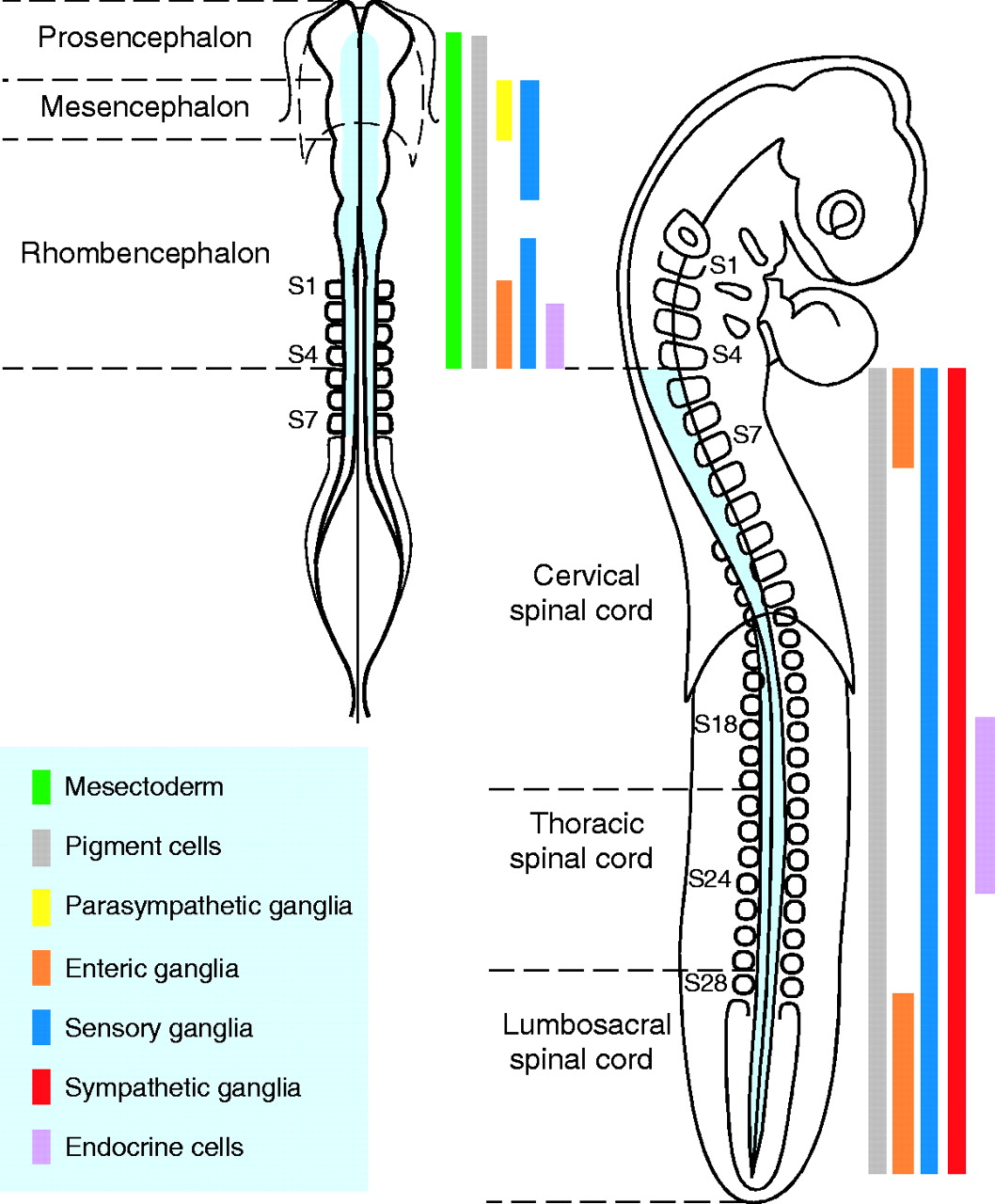
Definition – motor disorder of the intestines due to failure of the neural crest cells, which are precursors of ganglion cells) to fully migrate during embryonic development of the colon.

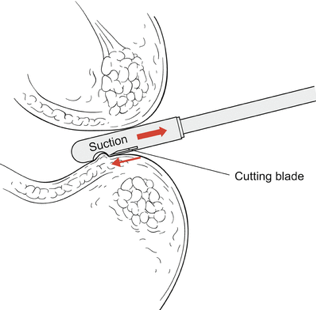
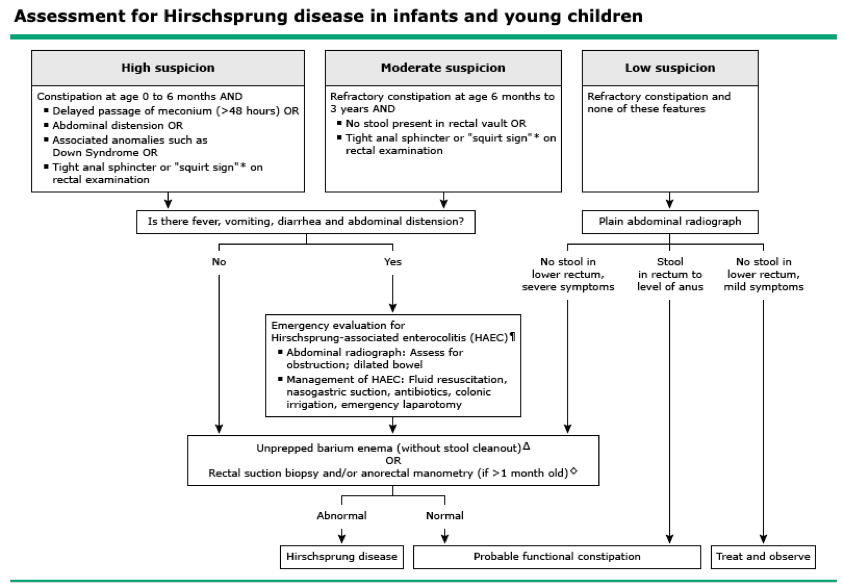
Clinical Significance – As a result of this aganglionosis of the colon, the distal intestines are unable to relax and cause a functional obstruction. Children affected by this condition fail to pass their meconium stool in the first 48 hours of life and may have abdominal distention, bilous emesis, and/or enterocolitis. Diagnosis is made with contrast enema and suction rectal biopsy.
History – Named after Harald Hirschprung (1830-1916), who was a Danish physician and received his medical doctorate from the University of Copenhagen in 1855. In 1870, he became the first Danish pediatrician and was appointed chief physician of Queen Louisa Hospital for Children in 1879. He presented his eponymous findings at the Berlin Congress for Children’s Diseases in 1886 where he described two infants who had died from “constipation associated with dilation and hypertrophy of the colon”. He published his findings a year later in an article entitled “Stuhlträgheit Neugeborener in Folge von Dilatation und Hypertrophie des Colons”. Other notable contributions of Dr. Hirschprung include being one of the first physicians to successfully reduce intussuception by pneumatic means and being an advocate for free health care for all children.

References
*** LISTEN TO THE PODCAST HERE ***
Pathophysiology

Epidemiology
Associated Syndromes
Associated Congenital Anomalies
Up to 25% of Hirschsprung patients have other congenital anomalies including:
Signs and Symptoms
Diagnostic Work-Up


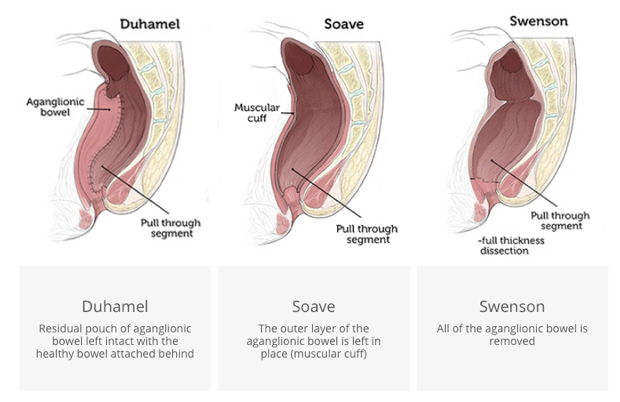
Treatment
The Cottage Physician (1893)

References
Question
You are consulted to see a 2-day old baby boy for failure to pass the first meconium stool and an episode of bilious emesis. He was 37-weeks gestation at the time of a normal spontaneous vaginal delivery without any complications. Physical examination reveals a distended abdomen and digital rectal exam results in an explosive expulsion of stool and gas. A contrast enema was ordered and is attached. What is the specific cause (not the diagnosis) of this infant’s condition and what is the next diagnostic step?

Answer
This infant has congenital aganglionic megacolon, or Hirschprung Disease. It is caused by the failure of the neural crest cells (precursors to enteric ganglion cells) to migrate completely during intestinal development in utero. This results in the failure of the colon to be able to relax and causes a functional obstruction.
Diagnosis is made with bedside suction rectal biopsy 2cm above the level of the dentate line. Confirmatory findings on histology are abnormal acetylcholine esterase-positive nerve fibers in the mucosa.

Sphincter of Oddi
Other known aliases – hepatopancreatic sphincter, Glisson’s sphincter
Definition – muscular ring surrounding the major duodenal papilla at the 2nd portion of the duodenum.

Clinical Significance – the sphincter of Oddi allows for drainage of the biliary and pancreatic systems and dysfunction (mainly spasming) can can cause pancreatitis. It is in a constant state of contraction unless relaxed by cholesytokinin released by vasoactive intestinal peptide. Opioids, specifically morphine, has been shown to increase the risk of sphincter of Oddi dysfunction.
History – Named after Ruggero Ferdinando Antonio Guiseppe Vincenzo Oddi (1864-1913), who was an Italian physiologist and anatomist from Perugia. He spent is formative years studying medicine at Perugia, Bologna, and Florence and was appointed head of the Physiology Institute at the University of Genoa in 1894. In 1887, at only 23 years old, he described his eponymous structure in his paper “D’une disposition a sphincter speciale de l’ouverture du canal choledoque”. His career, unfortunately, was derailed and cut short due to opioid addiction many believe was as a result of using morphine derivatives to study dysfunction of the sphincter.


References
Question
For celiac disease:
Answer
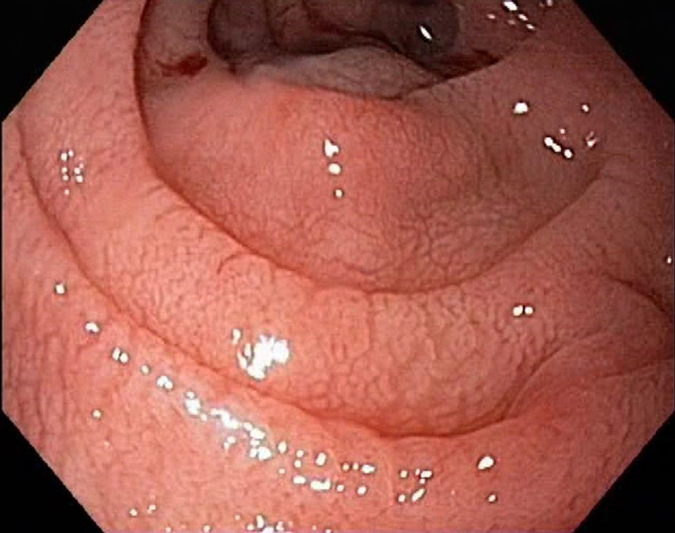
Initial screening test for suspected celiac disease is a serum immunoglobulin A (IgA) anti-tissue transglutaminase (TTG). If positive, it is then followed up with an endoscopic duodenal biopsy.

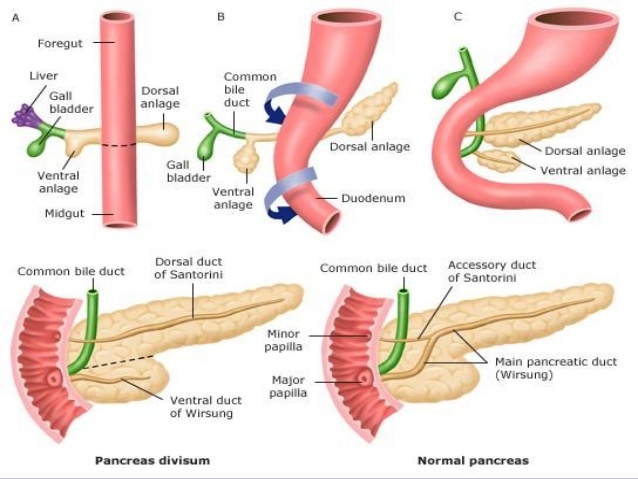
Duct of Santorini
Other known aliases – accessory pancreatic duct
Definition – portion of the dorsal duct distal to the dorsal-ventral fusion point during embryonic development
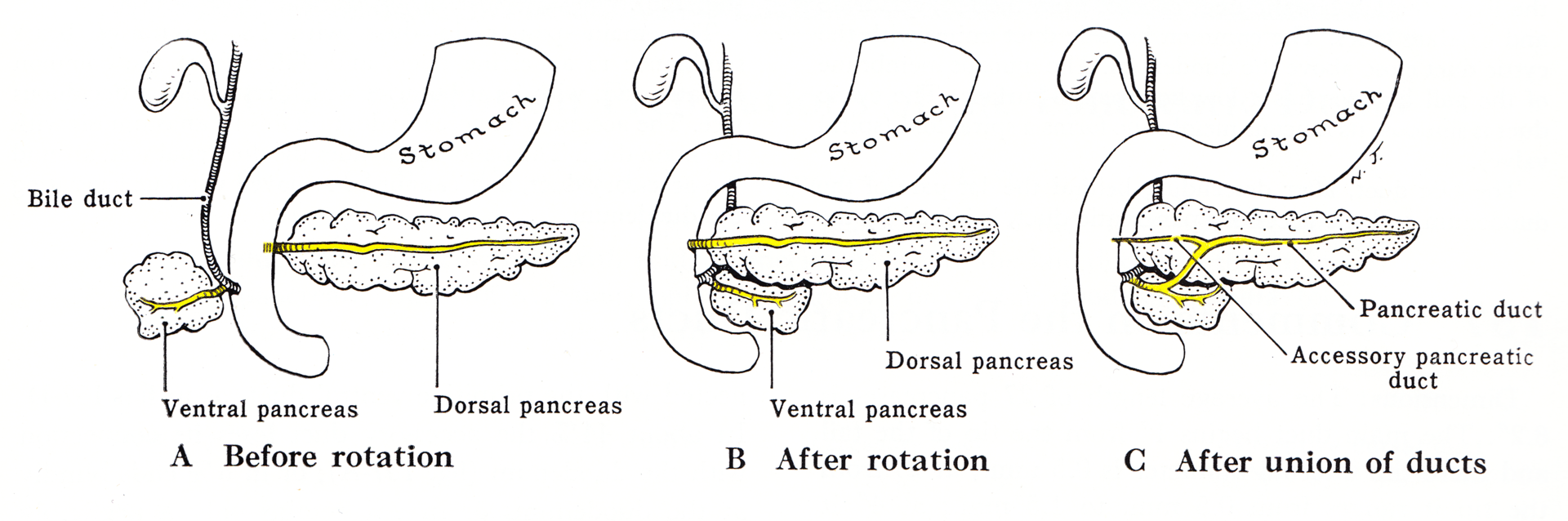
Clinical Significance – 85% of the population have a single, main pancreatic duct and 15% can have an accessory duct that either drains into the duodenum by a separate ampulla (2/3), or drains into the main duct (1/3). These anatomical variants need to be explored prior to instrumentation for pancreatic pathology as it can occur with pancreas divisum, which makes the accessory duct the principle drainage duct for the pancreas.
History – Named after Giovanni Domenico Santorini (1681-1737), who was an Italian anatomist and son of an apothecary. He spent his formative years studying medicine throughout Bologna, Padua, and Pisa, where he received his medical doctorate in 1701. He performed anatomical dissection demonstration in Venice for 23 years, during which he published his most famous work entitled Observationes Anatomicae. This work was considered one of the most detailed and important anatomical texts of the time and gave way to descriptions of twelve different anatomic eponyms accredited to Santorini.

References
***LISTEN TO THE PODCAST HERE***
History of the Disease
The term “celiac” has Latin and Greek roots as Aretaeus of Cappadocia named this disease in the 1st century AD “koiliakos” meaning abdomen/abdominal in patients with chronic diarrhea. The first modern medical description of the disease was in 1888 by Samuel Gee in an paper entitled “On the Coeliac Affection”. The specific medical term for Celiac Disease is “gluten-sensitive enteropathy”. It was still relatively unexplained until Willem Dicke, a Dutch pediatrician, noted improvement in his patient’s abdominal symptoms during bread and grain shortages of World War II.
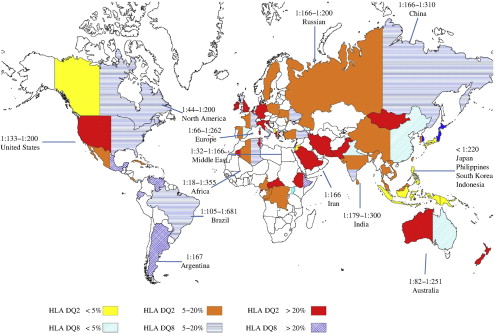
Epidemiology

Pathophysiology
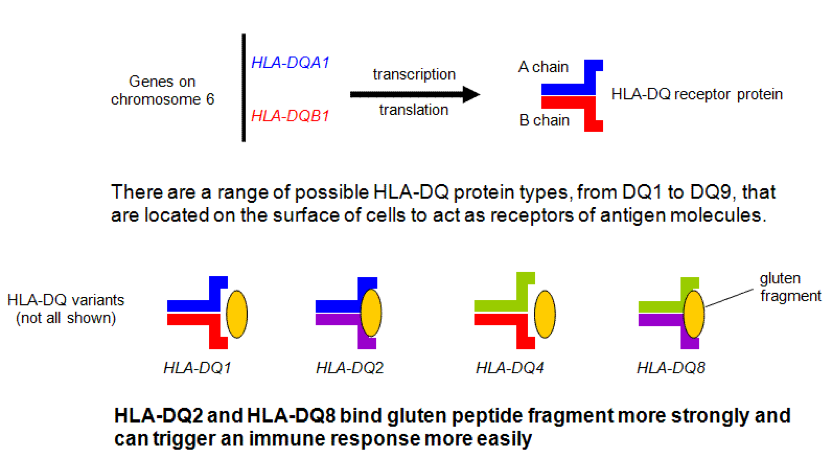
High association with genetic predisposition to gluten sensitivity, specifically HLA-DQ2 and/or DQ8, and because of these genetic changes, serum autoantibodies are produced that attack the endomysium of the enterocytes of the small bowel.
Signs and Symptoms
Originally thought to be a disease of infancy, it is being diagnosed later and later in life, with adults first being diagnosed as late as the fifth decade. Often, this is in the setting of failure to thrive in an infant.
Common
Associated Clinical Findings
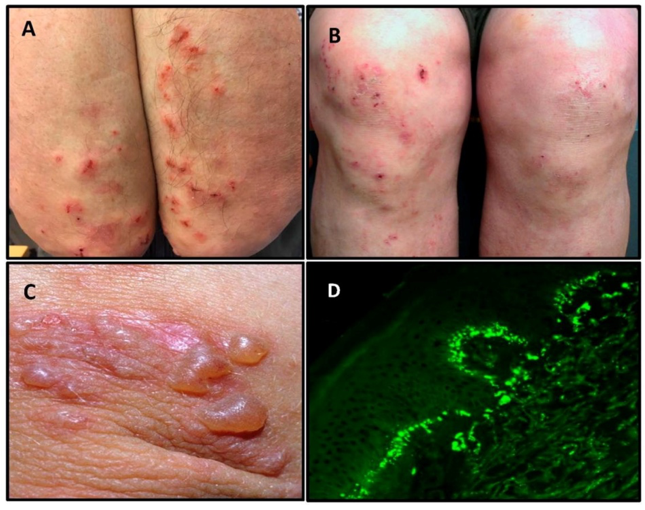
Screening and Diagnosis


Classification
Celiac disease can present as a spectrum of signs and symptoms and thus, have different classifications.
Management
Six key elements of successful management of celiac disease and it has a nice acronym:
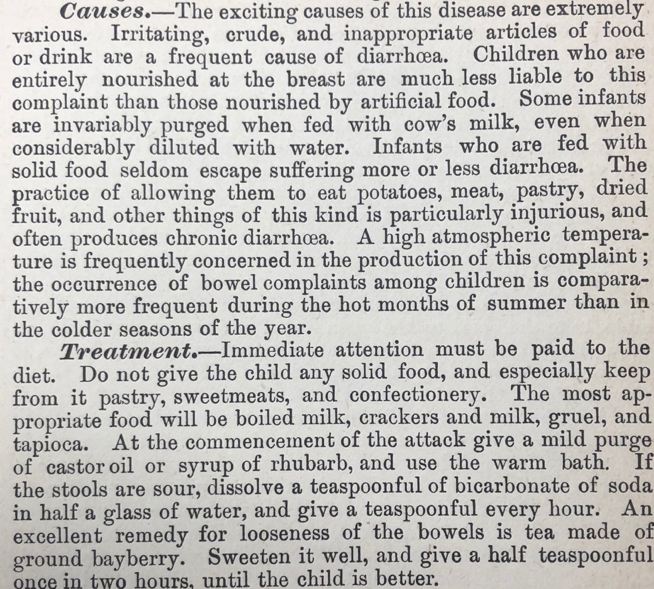
Cottage Physician
This is an excerpt from the pediatric disease section on diarrhea:
References